Diagnosis challenges and “not being taken seriously”
Why fibromylagia is not an acceptable diagnosis – you need to get clear about what fibro isn’t so you can find out what it really is (an “I don’t know” diagnosis) so that you can continue to explore what’s really behind your chronic illness
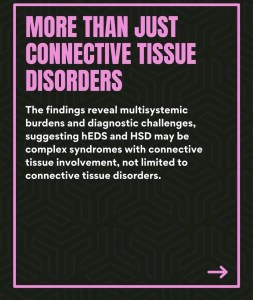
Hypermobility is a multi-systemic condition

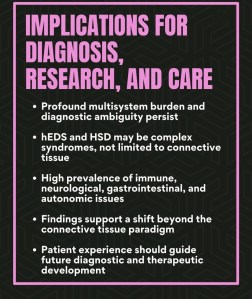
Screenshots with credit to The Norris Lab
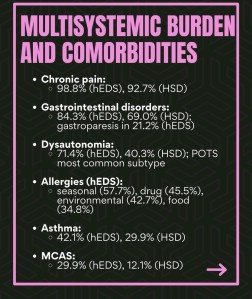
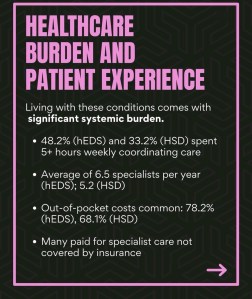
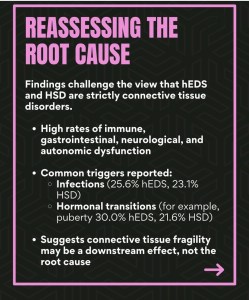
Groundbreaking new study: The Norris Lab has released one of the largest international surveys ever conducted on hypermobile Ehlers-Danlos Syndrome (hEDS) and Hypermobile Spectrum Disorders (HSD). By challenging some of the pre-existing ideas this will hopefully lead to improved clinician understanding and better outcome for patients. Highlights include:
- An average 22-year diagnostic delay for hEDS
- High rates of misdiagnosis, even under current criteria
- Multisystemic burdens spanning immune, neurological, gastrointestinal and autonomic systems
- A high prevalance of Postural Orthostatic Tachycardia Syndrome (POTS), Mast Cell Activation Syndrome (mCAS) and allergic-type conditions
- Significant out-of pocket costs and healthcare strain
- Evidence that hEDS and HSD may be complex syndromes, not just connective tissue disorders.
“Joint hypermobility may also be associated with an exaggerated fight-or-flight reaction. Eccles and her colleagues recently found support for this idea in a study of 400 psychiatric patients. They uncovered a simple yet powerful mechanism behind the link: the collagen abnormalities that make joints especially flexible seem to affect blood vessels, making patients prone to an accumulation of blood in the veins of the legs. This pooling may lead to exaggerated cardiovascular responses to maintain the output of blood from the heart. When the heart has to work extra hard just to circulate blood, it brings the entire body to the verge of a fight-or-flight reaction, requiring very little to set off panic”. Article in Scientific American.
Another new study Hypermobile Ehlers-Danlos Syndrome: Cerebrovascular, Autonomic and Neuropathic Features, the largest hEDS study to date (2025) also indicates that it is a multi-systemic complex condition. Key findings:
- 79% had reduced cerebral blood flow when upright, providing an explanation for dizziness and “brain fog.”
- 90% had signs of autonomic dysfunction (issues with heart rate, sweating, digestion).
- 64–82% showed small fiber neuropathy, linked to pain, numbness, and tingling.
- Tilt table testing revealed overlapping diagnoses, including POTS, cerebral hypoperfusion, and orthostatic hypotension.
- Only 33% met the criteria for POTS or postural orthostatic tachycardia syndrome (but, my note, what about all the other dysautonomias that get commonly missed).
Other relevant studies:
Joint hypermobility links neurodivergence to dysautonomia and pain
Autism/ADHD and overlapping chronic conditions
For the many resources relating to the cross-over of chronic health conditions with autism and ADHD, see separate Neurodiversity Resources page.
Autism and chronic illness: is there an overlap? – video
Joint hypermobility links neurodivergence to dysautonomia and pain
Risks of Fluoroquinolones (antibiotics) for people with Ehlers Danlos or connective tissue disorders
Medications to avoid with Ehlers-Danlos Syndrome: Fluoroquinolones
Also known as a “floxacin†antibiotics. This happened to me: just two doses of a “flox†antibiotic for a kidney infection triggered a severe adverse response following which neurological issues such as neuropathy became significantly and permanently worse and laxity became much more problematic.
Symptom Tracking and Recognition
Visible – an app for tracking symptoms and daily variables, specifically designed for invisible conditions, not for athletes!
Garmin watches – a link to the Venu which I used to track stress, body battery, HR and so on
HeartMath device – for tracking HRV, which can help get your ANS back on the level
Podcast episode discussing the value of using activity tracking devices
Hidden Disabilities Sunflower – ID cards and other resources bearing the sunflower symbol that you can self-purchase and wear to get recognised, and helped, as someone with a hidden disability
The National Disability Card UK – validated Disability Card with multiple benefits besides providing increased visibility and being a powerful self-advocacy tool
Nervous System Support
Smoveys for general rehab and nervous system resetting
Wilbarger Therapy Brush for sensory processing issues and sensory defensiveness
Loop earplugs designed especially with noise sensitivity, autism, ADHD and misphonia in mind, with various levels of noise reduction to suit different environments and social engagements. I never go anywhere without mine!
Various vagus nerve stimulation devices now available (expect a personalised response and requires trial and error so check return/refund terms before purchasing!)
Neck fan (various brands) – affordable devices, useful for temperature regulation with dysautonomias including POTS (am convinced they partly act as vagus nerve stimulation)
Bose Quiet Comfort earphones with ANC (useful with or without sound!)
Woolroom beds and bedding – great for temperature regulation, non-toxic sleep environment, natural comfort and joint support
What some of us already know “revealed” in a study…people who regularly pick up their craft, be it a needle, knitting or paintbrush aren’t just happier, they also feel life is more meaningful. It makes more difference to their sense of purpose than whether they had a job – Creating arts and crafting positively predicts subjective wellbeing.
Covid-19 and Long-Haul Covid Resources
Variant connective tissue as a risk factor for Long COVID: a case-control study
Energy medicine routine fo Vaccination Alignment and Integration by Prune Harris. This free routine, for pre and post vaccination, helped support me through my covid vaccination with no side effects (even with a history of reacting to vaccinations)!
Coronavirus Recovery – a course from Prune Harris
Discover how The Gupta Program can support your recovery from “Long-Haul Covid”.
Long-haul covid recovery using neuroplasticity.
Also see glutamates heading below.
Information related to supplements
Vitamin B1 (thiamine) as a mega dose – see my various posts on this topic:
Mega-dose Thiamine: Beyond addressing deficiency
Thiamine, Fibromyalgia and Chronic PainThiamine for EMF Sensitivity
Thiamine for nerve damage, trigeminal damage and hearing loss
EO Nutrition for multiple resources on this topic
12 Ways You Can Get Vitamin B1 (Thiamine) Deficiency
Vitamin B1 (Thiamine) Deficiency: The “Great Imitator” of other Illnesses
7 Unusual Vitamin B1 Deficiency Symptoms
Electrolytes: essential for POTS management: I use LMNT sugar/sweetener and additive free and sodium loaded – LMNT
Trudy Scott of Every Woman Over 29– topics related to use of amino acid supplements
B6 toxicity? Too much of a “good thing” is something else to consider when you are sensitive: B6 (pyridoxine) toxicity from taking too many supplements or drinks containing vitamin B6 has been associated with a range of unpleasant symptoms including, small fibre polyneuropathy which, in turn, can be an underlying cause of POTS (postural orthostatic tachycardia) and other dysautonomias. Other side effects can be dizziness, photosensitivity, sensory anomalies such as “glove and stocking” sensations on limbs, allodynia etc, involuntary movements, cramps, cold hands and feet, loss of bladder control and bladder pain, brain fog, breathing issues, nausea and acid reflux, amongst others (the actual list of associated symptoms is very long). In fact, as a known neurotoxin, B6 can get stored in muscle tissue, damaging nerve fibres along the way and so cause a perfect storm of autonomic and other issues. The recommended daily intake is very low (eg. 1.5mg per day for women over 50) compared to the typical doses found in supplemental products (often as much as 100mg) or various food products and sports drinks.
B6 Toxicity – Hemminger & Willis
Pyridoxine Toxicity Small Fiber Neuropathy With Dysautonomia: A Case Report – Bacharach, Lowden & Ahmed
Understanding B6 Toxicity – information including a protocol for detoxification
Article in the Guardian on this topic, 4th Jan 2025 – Simon never linked the pain in his hands and feet to multivitamins – but a pathology test did “A growing number of consumers are presenting with symptoms linked to high levels of vitamin B6, pathologists say, while the supplement industry goes unpoliced”.
Low Dose Naltrexone
Do your research and perhaps consider a trial of this “wonder” med which may help with multiple aspects of these chronic overlapping conditions. Essential resources to explore:
The LDN Book – volumes 1, 2, 3 & 4
The LDN Radio Show with Linda Elsegood
The LDN Trust website
The LDN research Trust facebook group for real life feedback and discussion
Books
Classic Pacing for a Better Life with ME – Ingebjørg Midsem Dahl
What is an EDS flare-up? (this article outlines the possible triggers, many of which overlap with ME/CFS and POTs, and ways to avoid
The Spontaneous Healing of Belief – Gregg Braden
The Spiritual Anatomy of Emotion: How Feelings Link the Brain, the Body, and the Sixth Sense – Michael A Jawer
The Highly Sensitive Person – Dr Elaine Aron
The Biology of Belief – Dr Bruce Lipton
Waking the Tiger: Healing Trauma: The Innate Capacity to Transform Overwhelming Experiences – Peter Levine
Burnout: The secret to solving the stress cycle – Emily Nagoski and Amelia Negowski
The Endorphin Effect: A breakthrough strategy for holistic health and spiritual wellbeing – William Bloom
CFS Unravelled: Get Well By Treating The Cause Not Just The Symptoms Of CFS, Fibromyalgia, POTS And Related Syndromes – Dan Neuffer
Weather and seasonal effects on chronic symptoms and pain
Pain and weather associations – Action mechanisms; personalized profiling
The October Slide: Managing Symptom Flare-Ups in the Fall EDS Clinic
Preparing for the October Slide with Chronic Illness throughfibrofog.com.
The October Slide: Chronic Illness Flares in the Fall, NormaLyte.
Blame it on the weather? The association between pain in fibromyalgia, relative humidity, temperature, and barometric pressure. PLoS ONE. 2019.
Influence of Weather on Daily Symptoms of Pain and Fatigue in Female Patients With Fibromyalgia. Arthritis Care Res. 2013.
Life event, stress and illness. Malaysian Journal of Medical Sciences. 2008.
Local weather is associated with rates of online searches for musculoskeletal pain symptoms. PLoS ONE
Oxalates
Sally K Norton’s website full of oxalate resources
Low Oxalate Diet Information – extremely useful resource including food lists, with associated Facebook support group TLO (Susan Owens manages both)
Elliot Overton website and blog, numerous articles and resources on oxalates
Oxalates Control is a major new factor in autism therapy – The Great Plains Laboratory, Inc.
How Oxalates Ruin Your Health – Interview (transcript) with Dr William Shaw
The Damaging Effects of Oxalates on the Human Body – Mercola
Low Oxalate Low Histamine Diet – The Missing Link? – Healing Histamines
How to Succeed At Reducing Oxalate on a Gluten-free Diet – a really helpful article, including adapting your flours
SHOUT OUT about Oxalates. Good news – Ehlers-Danlos Syndromes – a really positive outcome, and some advice, from someone with EDS who tried the low oxalate diet
Joint pain? Inflammation? Slow to heal? Fatigue? Sleep issues? – Sally K Norton
Glutamates
Glutamates and OCD:
Two independent groups from the University of Toronto and the University of Chicago published evidence in 2006 that a protein that carries glutamate in the brain is linked to OCD in some cases; more recent studies from groups at the Massachusetts General Hospital and Johns Hopkins University have found the same thing. Although it is not yet clear whether these genetic linkages correspond to a functional problem with this protein, problems with these glutamate transporters can increase the amount of glutamate found outside neurons, which might explain the increased glutamate seen in the brain, and possibly lead to OCD symptoms.
We worked with a patient with OCD who improved significantly after we added NAC to her existing medications. Unpublished clinical experience, from our group and elsewhere, further suggests that the agent may be of benefit in at least some patients with OCD. Well controlled studies have shown benefit from NAC in a variety of other disorders of compulsive and impulsive behaviors, including pathological gambling, Trichotillomania, and drug craving. Because it is inexpensive, has no significant side effects, and is available over-the-counter, this drug is a potentially attractive therapeutic option, though the evidence for benefit in OCD remains extremely thin. Taken from: New Horizons in OCD Research and the Potential Importance of Glutamate. Can We Develop Treatments That Work Better and Faster?
Glutamates and pain:
The role of glutamate signaling in pain processes and its regulation by GCP II inhibition
Glutamates and long covid:
* Brain MRI scans from people with ME/CFS and long COVID were analysed to measure levels of neurochemicals including glutamate (a neurotransmitter) and N-acetyl-aspartate (NAA; which has a number of functions).
* Glutamate levels in the brain were increased in ME/CFS and long COVID patients, while NAA levels were increased in long COVID.
* In both patient groups, neurochemical levels correlated with the severity of symptoms such as physical function, cognitive impairment, unrefreshing sleep and pain.
* Glutamate and NAA levels may therefore contribute to the complex symptoms experienced by people with ME/CFS and long COVID, while the similar patterns in both diseases support a possible overlap in their underlying pathology.
* The researchers will follow up this work by tracking progression of these and other brain abnormalities over time.
From Increased brain neurochemical levels in ME/CFS and long COVID
Long covid science that is emerging
Researchers in Japan have investigated why so many people with long COVID suffer from brain fog, meaning problems with memory and concentration. Brain fog is one of the most common symptoms, affecting more than 8 out of 10 people with long COVID, often with a major impact on daily life and work. The researchers suspected that brain fog might be linked to changes in AMPA receptors, which are key molecules for memory and learning in the brain. Using a new brain imaging technique, they were able to measure these receptors directly in living brains. They compared 30 people with long COVID and brain fog to 80 healthy individuals. The results showed that those with long COVID had significantly more AMPA receptors in the brain, and the higher the receptor levels, the worse the cognitive problems. They also found that elevated levels of inflammation were associated with the increase in receptors. How do AMPA receptors link to increased excitatory behaviour and/or brain fog? AMPA receptors are ligand-gated ion channels that mediate fast excitatory neurotransmission in the brain, acting as the primary transducers of signals from the neurotransmitter glutamate. They are the main “fast” signaling elements at synapses, transmitting rapid excitatory signals that underpin much of brain activity. They are crucial for higher brain functions, including learning and memory, through their involvement in synaptic plasticity, the mechanism underlying these cognitive processes.
The researchers emphasize that brain fog in long COVID should be recognized as a real clinical condition, not just a vague symptom. From my own personal experience of long covid, both increased overall brain fog and increased (frequency) and more intense (harder to mitigate, persistent and lasting) excitability phases have been the effects since contracting the virus 18 months ago.
New study reveals molecular basis of Long COVID brain fog
Systemic increase of AMPA receptors associated with cognitive impairment of long COVID
Autism and ADHD resources
See separate neurodivergence menu header
Low EMF, flicker-free SAD lamps and blue light blocking lights
Useful apps
Calm app – audio resources for sleep, soothing and meditation
Curable app – remarkably effective education resources and tools for chronic pain and anxiety
Effect of space weather on human biology
A possible association between space weather conditions and the risk of acute coronary syndrome in patients with diabetes and the metabolic syndrome – International Journel of Biometerology
Superposed epoch analysis of physiological fluctuations: possible space weather connections – International Journel of Biometerology
Long-Term Study of Heart Rate Variability Responses to Changes in the Solar and Geomagnetic Environment – Abdullah Alabdulgader, Rollin McCraty, Michael Atkinson, York Dobyns, Alfonsas Vainoras, Minvydas Ragulskis,and Viktor Stolc
Influence of electromagnetic fields on the circadian rhythm: Implications for human health and disease – Biomedical Journal
“Increase in cosmic rays, solar radio flux, and Schumann resonance power was all associated with increased HRV and parasympathetic activity. The findings support the hypothesis that energetic environmental phenomena affect psychophysical processes that can affect people in different ways depending on their sensitivity, health status and capacity for self-regulation.”
Highly Sensitive Person Resources
See seperate menu header for more HSP links and recommendations
Highly Sensitive Person website (resources including self-test, compiled by Dr Elaine Aron, author of The Highly Sensitive Person)
National Centre for High Sensitivity (UK)
The Highly Sensitive Person – Dr Elaine Aron
Quiet: The Power of Introverts in a World That Can’t Stop Talking – Susan Cain
Introvert, Dear – for Introverts and Highly Sensitive People
Sensitive: the Untold Story – Elaine Aron and featuring Alanis Morrissette
YouTube playlist of Highly Sensitive resources
Ehlers Danlos & Hypermobility Resources
The Zebra Club – Jeannie di Bon (very highly recommended movement practice for hEDS and HSD
Chimera Health – hypermobile fitness online tuition
The Bendy Bodies – podcast with Dr Linda Bluestein
Hypermobility Doctor – very useful Instagram account
The Hypermobile Syndromes Association
When to suspect EDS (in the context of fibromyalgia; an article similar viewpoint to my own)
Dr Jennifer Eccles resources – Dr Eccles and team have published papers recently demonstrating brain-body links between neurodivergence, emotion regulation and proprioception (read more here) and the role of neurodivergence and inflammation on chronic fatigue in adolescents (read more here). Alongside colleagues from Kings College London they published the first study linking hypermobility to Long Covid (read more here). In 2024 Dr Eccles was the winner of the Research Pioneer Award conferred by The Ehlers Danlos Society for her hypermobility research.
Mast Cell Activation Resources
When to Suspect MCAD (Mast Cell Activation Disorder) – a common co-condition of hEDS
Beth O’Hara – Functional Naturopath and Functional Genetic Analyst
ME / CFS Resources
ME/CFS may exist as a stand alone condition or be a co-condition with hEDS. Here are some resources I have found useful:
Classic Pacing for a Better Life with Me – Ingebjørg Midsem Dahl, very highly recommended handbook of pacing to manage ME/CFS (the most useful book I have found with many positive reviews)
The Chronic Fatigue and Burnout Recovery Podcast – a mine of useful information from Anna Marsh
Phoenix Rising – community and resources
The many challenges of living with ME/CFS
Quoted from “My full reality: the interim delivery plan on ME/ CFS”:
“The content described in the table below was collected through a small informal survey conducted with members of the ME Research Collaborative Patients Advisory Group and the ME/CFS Alliance. Representatives of Doctors with ME have also contributed. The content is not intended to represent the views of all people with personal experience of ME/CFS nor to represent all views that may be relevant.”
Issues reported on language used in relation to ME/CFS
| Issue | Why this is a problem to someone who has ME/CFS | What people say that is distressing or frustrating |
|---|---|---|
| Chronic fatigue syndrome – as an alternative description of ME/CFS | Chronic fatigue is only one of the many symptoms that people with ME/CFSexperience on a daily basis. The emphasis on this one symptom leads to misconceptions about the condition and how disabling it can be. Many people misunderstand the term ‘chronic fatigue’ as meaning ‘very tired’, but anyone can feel tired, without them being ill. This makes it harder to explain to others what the impact of ME/CFSactually is and why more sleep isn’t an answer. Fatigue is also a common symptom for many chronic illnesses. Emphasising chronic fatigue can lead to other symptoms being ignored. | Just go to bed earlier. I’d love it if I could stay in bed all day. You’re just lazy. Yeah, I’m very tired too. Sounds like a normal life (as a parent). I didn’t think it was a very serious condition. ME/CFS is fatigue or Tired All The Time (TATT). ME/CFS is deconditioning. |
| Normal experience of illness is that people recover | Some people with ME/CFS have low expectations of full recovery and prefer to minimise the severity of their symptoms or preventing deterioration by managing their life carefully. It can be distressing and frustrating when other people assume that recovery can be expected, when there is very little scientific evidence to show that this is the case. | You’ve just got to get more active. I don’t see why she doesn’t recover. My mum’s friend had that and she recovered. You’ll be fine. You should aim for full recovery. We can get you back to normal with some time and effort. The treatment works well, you have to change your idea of what recovery is. |
| The misconception that ME/CFSis a mental health condition, ‘all in the mind’ or that you can get better or overcome symptoms by the way you think | The World Health Organization classified ME/CFS as a neurological condition in 1969. Subsequent research and NICE guidance describe ME/CFSas a ‘complex, chronic medical condition affecting multiple body systems’. ME/CFS has never been classified as a mental health condition, but some clinicians choose to treat it that way. | Everyone’s been struggling since the pandemic. Are you sure it’s not health anxiety? Maybe you should ask your doctor to put up your dose of antidepressants. If you thought differently, you would get better. You need to make more of an effort. It helps to have a positive attitude. |
| The fact that there is no medical test to prove that someone has ME/CFS | As yet, there are no diagnostic tests to show when someone has ME/CFS. This is because there hasn’t been enough research to explain the causes and how to test for the condition. This isn’t the fault of the person with ME/CFS but they can be made to feel that they are lying or seeking unnecessary attention. Alternatively, people can spend a long time being sent to different specialists to rule out other options. Tests in themselves are not bad, and conversely, many patients are not offered tests because clinicians don’t take their symptoms seriously or assume that, if they have ME, there’s no need to look further. The problem is that participating in testing can be exhausting and often delays diagnosis. | The test results came back normal so: – you need to be referred to another specialist – I can’t find anything wrong with you – you are lying – maybe you are depressed about something – good news – the tests say there is nothing wrong with you – you can’t really be sick, because one of these tests would show something |
| ‘Post-exertional malaise’ or PEM is a technical term which most people will not have heard of | PEM is one of the 4 key features of ME/CFSaccording to the NICE guideline on ME/CFS(NG206). It can be hard to explain. ‘Exertional’ means all activity – physical, cognitive, social, and emotional. The negative effects can be both immediate and/or longer term. The effect can also be delayed after the initial trigger. | You did nothing yesterday, why are you still in bed? |
| Symptoms of ME/CFScannot be seen | The invisible nature of ME/CFSmeans that it can be hard for other people to accept there is anything wrong, particularly in people with mild or moderate symptoms. ME/CFS does not cause obvious visible physical differences. People with ME/CFS who are housebound can become invisible to society as they are rarely, if ever, seen, including by clinicians. With severe ME/CFS, people can be bedbound, tube-fed and only leave their homes in an emergency. The effects of the illness can be visible, but the people with these symptoms are rarely seen. | You look normal. You just don’t want to work. Have you just tried eating better? Is it as bad as you say it is? You don’t need the wheelchair because I saw you walk last week. Of course you can walk, you don’t have a broken leg or anything. No, you can’t have a home visit. |
| People with mild or moderate ME/CFS can manage their energy to do something out of their ordinary routine, as long as they rest before and afterwards as necessary | Other people may not understand the need to manage or ‘pace’ daily energy supplies. This means that when they see the person with ME/CFS, they do not realise that they are seeing that person at their best. This can lead to misunderstanding and suspicion about whether the person is actually ill. When people with ME/CFS have severe symptoms, they cannot socialise or go out so others do not see the impact of the condition on them. | How can you go for lunch with someone, but you can’t go to work for 8 hours? You shouldn’t be going on holiday if you can’t work full time. You went for a walk yesterday – you don’t need that aid. The tests are only available in the mornings. We need you to commit to attending weekly. The equipment needs to be returned to us the day after the test. |
Further evidence about the experience of having ME/CFS
Action for ME, 2020. The Big Survey 2019 (last viewed on 2 May 2023).
Action for ME, 2017. Families facing false accusations: results of Action for ME’s survey. Available to download from Action for ME: support for parents (last viewed 2 May 2023).
Action for ME, 2015. 2015 survey: ‘Close to collapse’. Available to download from Action for ME: support for social care professionals (last viewed on 2 May 2023).
‘Dialogues for a neglected illness’ funded by the Wellcome Public Engagement Fund (2018).
Kingdon, CC, Bowman, EW and others, 2018. ‘Functional status and well-being in people with myalgic encephalomyelitis/chronic fatigue syndrome compared with people with multiple sclerosis and healthy controls’. PharmacoEconomics Open 2, 381–392 (last viewed 3 May 2023).
Tripp C (2022). ‘Understanding ME and chronic fatigue syndrome in children’ (last viewed 5 May 2023).
- ME/CFS Research Review. Analysis of data from 500,000 individuals in UK Biobank demonstrates an inherited component to ME/CFS. 11 June 2018. ↩
- Pendergrast T, Brown A, Sunnquist M and others. ‘Housebound versus nonhousebound patients with myalgic encephalomyelitis and chronic fatigue syndrome’. Chronic Illness. December 2016. ↩
- Montoya JG, Dowell TG, Mooney AE, Dimmock ME, Chu L. ‘Caring for the patient with severe or very severe myalgic encephalomyelitis/chronic fatigue syndrome’. Healthcare. 2021. ↩
- Pheby DFH, Araja D, Berkis U, Brenna E, Cullinan J, de Korwin JD, Gitto L, Hughes DA, Hunter RM, Trepel D, Wang-Steverding X. ‘A literature review of GP knowledge and understanding of ME/CFS: a report from the socioeconomic working group of the European Network on ME/CFS’. Medicina (Kaunas). 24 December 2020. ↩
- Hng KN, Geraghty K, Pheby DFH. ‘An audit of UK hospital doctors’ knowledge and experience of myalgic encephalomyelitis’. Medicina (Kaunas). 27 August 2021. ↩
- Devendorf AR, McManimen SL, Jason LA. Suicidal ideation in non-depressed individuals: The effects of a chronic, misunderstood illness. J Health Psychol. Nov-Dec 2020. ↩
- Falk Hvidberg M, Brinth LS, Olesen AV, Petersen KD, Ehlers L. The health-related quality of life for patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). PLoS One. 6 July 2015. ↩
- Davis HE, McCorkell, L Vogel, JM and others. Long COVID: major findings, mechanisms and recommendations. Nature Reviews Microbiology (2023). ↩
- NIHR Themed Review: Living with COVID-19. October 2020. ↩
- Boulazreg S, Rokach A. The lonely, isolating, and alienating implications of myalgic encephalomyelitis/chronic fatigue syndrome. Healthcare (Basel). 20 October 2020. ↩
- Brittain E, Muirhead N, Finlay AY, Vyas J. Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): major impact on lives of both patients and family members. Medicina (Kaunas). 7 January 2021. ↩
- Nigel Speight. Severe ME in children. Healthcare (2020). ↩
Healing Protocols for Chronic Conditions
In my experience, these can be helpful to a degree but are not the panacea you may hope they will be versus (in some cases) the considerable cost of subscribing; so explore and take what resonates, leave the rest.
CFS Health – Help for ME/Chronic Fatigue Syndrome, Fibromyalgia, POTS, Long Covid, and Post Viral Fatigue
The Cure for Chronic Pain – Nicole Sachs, podcast, videos and courses
The Gupta Program – an approach for tackling chronic conditions
Anna Marsh – Functional Medicine and Fatigue Recovery (see related podcast below)
The Mindbody Prescription: Heating the body, healing the pain – Dr John Sarno
The Divided Mind: The Epidemic of Mindbody Disorders – Dr John Sarno
The Cure for Chronic Pain podcast and website
Disclaimer: This blog, it’s content and any material linked to it are presented for autobiographical, general interest and anecdotal purposes only. They are not a substitute for medical advice, diagnosis, treatment or prescribing. Opinions are my own based on personal experience. Please seek medical advice from a professional if you are experiencing any mental or physical symptoms that concern you.

